Tuesday, 31 December 2019
Thursday, 26 December 2019
Monday, 2 December 2019
Tuesday, 26 November 2019
Saturday, 23 November 2019
Thursday, 17 October 2019
Sunday, 6 October 2019
Saturday, 5 October 2019
Friday, 4 October 2019
Wednesday, 2 October 2019
Sunday, 22 September 2019
Saturday, 21 September 2019
Friday, 20 September 2019
Thursday, 19 September 2019
Wednesday, 18 September 2019
Saturday, 31 August 2019
Diagnosis of acute myocardial infarction in the presence of left bundle branch block
Specific ECG criteria in LBBB patients, including concordant
ST-segment elevation (criteria 1) or depression (criteria 2) or
pronounced discordant ST-segment elevation (criteria 3), in
specific ECG leads and an alternative ECG criteria, including
ST-segment depression or elevation discordant with the
QRS complex with a magnitude of at least 25% of the QRS
complex (alternative criteria 3), together with suggested
high-sensitivity cardiac troponin ((h)s-cTn) thresholds (eg,
hs-cTnT ≥42 ng/L at presentation), allow an accurate and
immediate triage to coronary angiography in patients with
LBBB and symptoms suggestive of AMI.
Original criteria
Modified criteria
ST-segment elevation (criteria 1) or depression (criteria 2) or
pronounced discordant ST-segment elevation (criteria 3), in
specific ECG leads and an alternative ECG criteria, including
ST-segment depression or elevation discordant with the
QRS complex with a magnitude of at least 25% of the QRS
complex (alternative criteria 3), together with suggested
high-sensitivity cardiac troponin ((h)s-cTn) thresholds (eg,
hs-cTnT ≥42 ng/L at presentation), allow an accurate and
immediate triage to coronary angiography in patients with
LBBB and symptoms suggestive of AMI.
Original criteria
Modified criteria
Saturday, 13 July 2019
Sunday, 7 July 2019
Saturday, 6 July 2019
Friday, 5 July 2019
Thursday, 4 July 2019
Wednesday, 3 July 2019
Thursday, 27 June 2019
Sunday, 23 June 2019
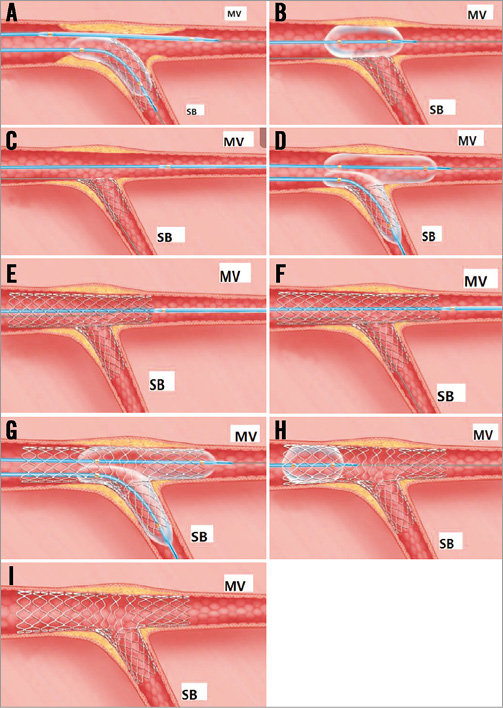
Drug-eluting or bare-metal stents for percutaneous coronary intervention
Drug-eluting or bare-metal stents for percutaneous coronaryintervention
We obtained individual data for 26616 patients in 20 randomised trials. Mean follow-up was 3·2 (SD 1·8) years. The risk of the primary outcome was reduced in DES recipients compared with BMS recipients (HR 0·84, 95% CI 0·78–0·90, p<0·001) owing to a reduced risk of myocardial infarction (0·79, 0·71–0·88, p<0·001) and a possible slight but non-significant cardiac mortality benefit (0·89, 0·78–1·01, p=0·075). All-cause death was unaffected (HR with DES 0·96, 95% CI 0·88–1·05, p=0·358), but risk was lowered for definite stent thrombosis (0·63, 0·50–0·80, p<0·001) and target-vessel revascularisation (0·55, 0·50–0·60, p<0·001). We saw a time-dependent treatment effect, with DES being associated with lower risk of the primary outcome than BMS up to 1 year after placement. While the effect was maintained in the longer term, there was no further divergence from BMS after 1 year.
We obtained individual data for 26616 patients in 20 randomised trials. Mean follow-up was 3·2 (SD 1·8) years. The risk of the primary outcome was reduced in DES recipients compared with BMS recipients (HR 0·84, 95% CI 0·78–0·90, p<0·001) owing to a reduced risk of myocardial infarction (0·79, 0·71–0·88, p<0·001) and a possible slight but non-significant cardiac mortality benefit (0·89, 0·78–1·01, p=0·075). All-cause death was unaffected (HR with DES 0·96, 95% CI 0·88–1·05, p=0·358), but risk was lowered for definite stent thrombosis (0·63, 0·50–0·80, p<0·001) and target-vessel revascularisation (0·55, 0·50–0·60, p<0·001). We saw a time-dependent treatment effect, with DES being associated with lower risk of the primary outcome than BMS up to 1 year after placement. While the effect was maintained in the longer term, there was no further divergence from BMS after 1 year.
Saturday, 22 June 2019
Monday, 17 June 2019
Tuesday, 23 April 2019
Saturday, 20 April 2019
Tuesday, 2 April 2019
Wednesday, 13 March 2019
Sunday, 10 March 2019
Friday, 8 March 2019
Saturday, 9 February 2019
Friday, 8 February 2019
Wednesday, 6 February 2019
Sunday, 3 February 2019
Sunday, 27 January 2019
Saturday, 26 January 2019
Tuesday, 22 January 2019
Monday, 21 January 2019
Mixed Type of Total Anomalous Pulmonary Venous Connection
Mixed Type of Total AnomalousPulmonary Venous Connection
 |
| Successful Surgical Management of a Rare Case of Mixed Type of Total Anomalous Pulmonary Venous Connection in a Very Low Birth Weight Preterm Child Using a Novel Surgical Technique |
Sunday, 13 January 2019
Friday, 11 January 2019
Definition of Infective Endocarditis (IE): Modified Duke Criteria
Definite Infective Endocarditis
Pathological Criteria
• Microorganisms demonstrated by results of cultures or histologic examination of a vegetation, a vegetation that has embolized, or an intracardiac abscess specimen; or
• Pathologic lesions; vegetation, or intracardiac abscess confirmed by results of histologic examination showing active endocarditis
Clinical Criteria
• 2 major criteria, or
• 1 major criterion and 3 minor criteria, or
• 5 minor criteria
Possible Infective Endocarditis
• 1 major criterion and 1 minor criterion or 3 minor criteria
Rejected Diagnosis of Infective Endocarditis
• Firm alternate diagnosis explaining evidence of suspected IE, or
• Resolution of IE syndrome with antibiotic therapy for ≤4 days, or
• No evidence of IE at surgery or autopsy, on antibiotic therapy for ≤4 days, or
• Does not meet criteria for possible IE
Definition of Terms Used in the Modified Duke Criteria for Diagnosis of Infective Endocarditis
Major Criteria
• Blood culture findings positive for IE
Typical microorganisms consistent with IE from two separate blood cultures:
• Viridans streptococci, Streptococcus gallolyticus (formerly known as S. bovis ), Staphylococcus aureus, HACEK group, or
• Community-acquired enterococci, in the absence of a primary focus, or
Microorganisms consistent with IE from persistently positive blood culture findings, defined as:
• ≥2 positive culture findings of blood samples drawn >12 hours apart, or
• 3 or most of ≥4 separate culture findings of blood (with first and last sample drawn ≥1 hour apart)
• Single positive blood culture for Coxiella burnetii or anti–phase I IgG titer ≥1 : 800
• Evidence of endocardial involvement
Echocardiographic findings positive for IE (TEE recommended in patients with prosthetic valves, rated at least possible IE by clinical criteria or complicated IE [paravalvular abscess]; TTE as first test in other patients), defined as follows:
• Oscillating intracardiac mass on valve or supporting structures, in the path of regurgitant jets, or on implanted material in the absence of an alternative anatomic explanation, or
• Abscess, or
• New partial dehiscence of prosthetic valve
New valvular regurgitation; worsening or changing of preexisting murmur not sufficient
Minor Criteria
• Predisposition, predisposing heart condition, or intravenous drug use
• Fever—temperature >38°C
• Vascular phenomena, major arterial emboli, septic pulmonary infarcts, mycotic aneurysm, intracranial hemorrhage, conjunctival hemorrhages, and Janeway lesions
• Immunologic phenomena: glomerulonephritis, Osler nodes, Roth spots, and rheumatoid factor
• Microbiologic evidence: positive blood culture finding but does not meet a major criterion as noted above (excludes single positive culture findings for coagulase-negative staphylococci and organisms that do not cause endocarditis) or serologic evidence of active infection with organism consistent with IE
Modified from Li JS, Sexton DJ, Mick N, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 2000;30:633.
Pathological Criteria
• Microorganisms demonstrated by results of cultures or histologic examination of a vegetation, a vegetation that has embolized, or an intracardiac abscess specimen; or
• Pathologic lesions; vegetation, or intracardiac abscess confirmed by results of histologic examination showing active endocarditis
Clinical Criteria
• 2 major criteria, or
• 1 major criterion and 3 minor criteria, or
• 5 minor criteria
Possible Infective Endocarditis
• 1 major criterion and 1 minor criterion or 3 minor criteria
Rejected Diagnosis of Infective Endocarditis
• Firm alternate diagnosis explaining evidence of suspected IE, or
• Resolution of IE syndrome with antibiotic therapy for ≤4 days, or
• No evidence of IE at surgery or autopsy, on antibiotic therapy for ≤4 days, or
• Does not meet criteria for possible IE
Definition of Terms Used in the Modified Duke Criteria for Diagnosis of Infective Endocarditis
Major Criteria
• Blood culture findings positive for IE
Typical microorganisms consistent with IE from two separate blood cultures:
• Viridans streptococci, Streptococcus gallolyticus (formerly known as S. bovis ), Staphylococcus aureus, HACEK group, or
• Community-acquired enterococci, in the absence of a primary focus, or
Microorganisms consistent with IE from persistently positive blood culture findings, defined as:
• ≥2 positive culture findings of blood samples drawn >12 hours apart, or
• 3 or most of ≥4 separate culture findings of blood (with first and last sample drawn ≥1 hour apart)
• Single positive blood culture for Coxiella burnetii or anti–phase I IgG titer ≥1 : 800
• Evidence of endocardial involvement
Echocardiographic findings positive for IE (TEE recommended in patients with prosthetic valves, rated at least possible IE by clinical criteria or complicated IE [paravalvular abscess]; TTE as first test in other patients), defined as follows:
• Oscillating intracardiac mass on valve or supporting structures, in the path of regurgitant jets, or on implanted material in the absence of an alternative anatomic explanation, or
• Abscess, or
• New partial dehiscence of prosthetic valve
New valvular regurgitation; worsening or changing of preexisting murmur not sufficient
Minor Criteria
• Predisposition, predisposing heart condition, or intravenous drug use
• Fever—temperature >38°C
• Vascular phenomena, major arterial emboli, septic pulmonary infarcts, mycotic aneurysm, intracranial hemorrhage, conjunctival hemorrhages, and Janeway lesions
• Immunologic phenomena: glomerulonephritis, Osler nodes, Roth spots, and rheumatoid factor
• Microbiologic evidence: positive blood culture finding but does not meet a major criterion as noted above (excludes single positive culture findings for coagulase-negative staphylococci and organisms that do not cause endocarditis) or serologic evidence of active infection with organism consistent with IE
Modified from Li JS, Sexton DJ, Mick N, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 2000;30:633.
Wednesday, 9 January 2019
Monday, 7 January 2019
Sunday, 6 January 2019
Saturday, 5 January 2019
HealthforHeart: Secondary prophylaxis to control rheumatic heart d...
HealthforHeart: Secondary prophylaxis to control rheumatic heart d...: Secondary prophylaxis to control rheumatic heart disease in developing countries: Put into a cage if can't be killed
Friday, 4 January 2019
Thursday, 3 January 2019
Subscribe to:
Comments (Atom)